This article begins with a story from my life, my fatherhood, about the time I was most afraid. The story ends happily with the birth of a healthy baby girl. The article, on the other hand, ends with an analysis showing how medical habit increased the threat to my daughter’s life by a factor of 20.
I learned the principals of acoustic imaging in my first professional job on an air-based passive sound imaging system, and on undersea sonar systems. These systems deal with inhomogeneous media, that is materials that aren’t the same throughout. The human body is an example of the inhomogeneous media, and ultrasound technicians are well aware of the challenges. The science of sonar has much in common with the science of ultrasound imaging.
At the end of June 2008 my wife was 27 weeks pregnant with our daughter. Her first pregnancy had been difficult because she had preeclampsia that deteriorated into HELLP syndrome around the time she was induced. Since the first pregnancy was medically complicated, the second pregnancy came with extra monitoring. She had more ultrasounds and more checkups than a typical pregnancy for a woman of her age.
She was given an ultrasound examination; I was there watching the screen. Part of the test included a cranial artery peak velocity measurement. This test was never prescribed, or at least we were later told there was no reason it should have been prescribed. Systolic flow is the fastest; it occurs when the heart contracts to push blood throughout the body. To measure the peak systolic velocity of blood flow in the middle cerebral artery, the technician puts the ultrasound in Doppler mode, and then carefully tries to hit a tiny moving target inside another person. That is, to hit a tiny moving target inside the person who is inside the person. The technician must align the ultrasound transducer’s boresight with the artery, to measure the Doppler flow accurately. This is a difficult ultrasound procedure. It took, if I recall correctly, about 15 minutes to generate the single peak velocity number.
Unfortunately, at 54 cm/s the flow rate was considered a strong indicator for for fetal anemia or hydrops. The prescribed treatment for fetal anemia is a transfusion. To give the transfusion a long needle is inserted through the mother’s abdomen, the uterus wall, and into the umbilical cord, where specially treated (irradiated) blood elements can be injected. Ultrasound is used to guide the needle in.
The procedure is risky. About 50% of the time the injection causes the umbilical cord to spasm, cutting off oxygen to the fetus. If this happens treatment is an emergency Caesarian and the delivery of a 27 week old premature baby. The prognosis for life at 27 weeks is about 90% according to babycenter. The same site indicates that 25% of those who live will have serious lasting medical problems—like cerebral palsy. An additional 50% will have some kind of lasting problem.
In my entire life I have never been as afraid, or worried, as I was through the day that followed that diagnosis. My initial reaction was skepticism. I demanded that the doctor defend the diagnosis, that she provide evidence to me that diagnosis was real and accurate.
It is well that I did.
I don’t remember every word I exchanged with the doctor. I can remember sitting in her office, across her desk. I can remember meeting each of her assertions with questions. I cannot remember being uncivil or rude, but I was terrified and may have been. I remember when she answered one of my questions with “I don’t tell you how to do your job!”
The hospital mobilized irradiated blood, and prepared an operating facility, and a prepped a sunny young doctor who had seen fetal transfusion performed (but not recently).
My daughter did not have hydrops.
I believe my skepticism saved the life of my daughter. I do not forgive that doctor. Mistakes happen, and even when bad, frightening things happen to me, I can forgive that. But I will never forgive her arrogance, the casual way she reached a conclusion and decided that nobody, especially the client, had the right to challenge her. May she find justice.
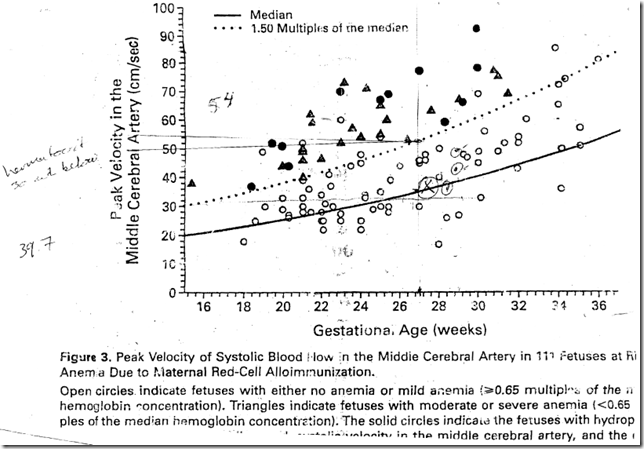
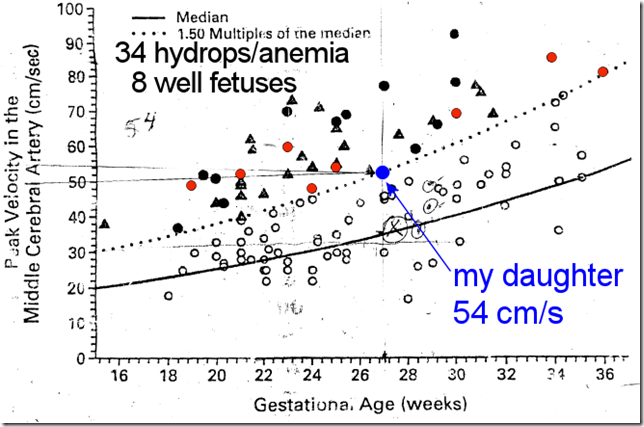
To her credit, she did eventually share some data with me. We walked together to one room, and she unpinned a photocopied graph from the wall. She took it to the photocopier and gave me a copy. This graph.
My questioning led them to delay the infusion by a day and to take an additional measurement. I watched the screen during the rest of the measurements. One ultrasound technician rotated the cart to block my view. I got up and walked around to see the screen. I challenged each of the technicians, and each of the doctors on the measurements. I pointed out that the measurement (54 cm/s) was on the threshold, not clearly over the threshold.
After the team of doctors and technicians finally decided that they could not repeat the high flow measurement, they continued looking. One doctor seized control of the transducer from the ultrasound technician and tried to examine my daughter’s thorax. She thought she could see a dark pocket (which could indicate hydrops). What she could see is a dark pocket, which in sonar is called a “shadow zone”. In this case the shadow zone appeared because the ultrasound had to pass obliquely through the fetus’s rib cage. The sound was refracted away from her abdomen leaving a dark region. The technician was appreciably better with the instrument than the physician.
The bull-dog tenacity was unbelievable. Given one incorrect diagnosis, the propensity to look, and look, and look for more problems is insane.
Analysis of Risk
Risk is a code word meaning that bad things might happen. It is calculated, usually, by counting the number of people to which bad things actually happened. Here I’ve annotated the graph with some numbers, I’ve marked my experience, and I’ve highlighted some samples. This is a very, very, small sample.
By my count there are 8 “well fetuses” whose peak velocity exceeds 1.5 times the median. There are 34 anemic fetuses, all of whose peak measurements exceeded the threshold. By those counts, if you get a high measurement then the odds you are actually sick are about 80% (34/42).
Prevalence of hydrops among the western first world population is quite low. In a study at a single hospital in Belfast, of 25,443 live babies 35 had fetal hydrops, or a prevalence of 1.34/1000. Presumably this excludes stillbirths, which in the U.S. account for 1 in 115 (much, much more prevalent than fetal hydrops live births). The best data I could find for the rate hydrops among stillbirths is from the Arizona Department of Health Services, which reported 6 of 158 still births to be due to, or coincident with, hydrops.
For purposes of this discussion, assume that:
- Hydrops affects 1.34/1000 live births
- 8.7/1000 are stillborn
- Of that 8.7/1000, Hydrops affects 3.8% of still births, or 0.33/1000 births
- Thus, hydrops has a prevalence among all pregnancies of about 1.67/1000
Prognosis if the fetus has hydrops is poor, with about a 90% morbidity rate according to Yong, a crude approximation that is still reasonable if accounting for non-immune and immune hydrops. The data I have is not very strong, rates vary wildly.
First, let us assume Eve has taken a break from her cryptanalysis work and is now pregnant. There is a small chance that Eve’s fetus has hydrops, 1.67/1000. Her physician sends her for an ultrasound. Due to poor handwriting her fetus is given a cerebral artery peak systolic Doppler ultrasound.
Suppose that Eve’s fetus has hydrops (she was part of the 1.67 of 1000). The ultrasound shows this correctly since there are no false negatives in the chart above. The doctors order a transfusion, which has all kinds of possible complications. We’ll ignore those complications, and just assume that Eve’s fetus has a 10% chance of survival—hydrops isn’t really very curable. She will spend a lot of money, and a lot of fear on procedures. It is not clear if these treatments change the outcomes at all (see, for example, Gynekol 1996 abstract).
Suppose that Eve’s fetus does not have hydrops, which is the much more likely case of 998.33/1000. The ultrasound correctly reports “no hydrops” 81% of the time (34 of 42 dots on the graph). Unfortunately, Eve is part of the other 19%, and the test says her fetus is hydropic. She follows her doctor’s stern council, and has an intrauterine transfusion. This is a gamble, and here are her odds (again from babycenter).
| Likelihood | Outcome |
| 4% | Caesarian, child dies |
| 10% | Caesarian, very bad health (e.g. cerebral palsy) |
| 21% | Caesarian, poor health |
| 11% | Caesarian, good health |
| 51% | Transfusion succeeds |
The main downside of a successful transfusion is cost, though there are probably rare cases of immune responses or transfusion induced illness. Eve’s cryptography work has grossed her lots of off-book income, so ignore the dollar cost of the operation. Furthermore, assume she does not contract MRSA in the hospital.
Eve had a test. If she had hydrops she changed the prognosis of her child almost none. If she did not have hydrops, she subjected herself and her fetus to really bad risks with no possible benefit.
Consider the population of Eves. Suppose that the doctors test every woman for hydrops. Disregarding the dollar cost, we have increased the risk of pregnancy so that 19% of pregnancies will result in hydrops treatments, of which 49% will result in very early preemies, of which 35% will have severe complications. In other words, testing has replaced the risk of hydrops (1.67/1000) with the risk of misdiagnosis and severe complications 32.6/1000. Testing every woman would increase the US infant mortality rate from 6.81/1000 to about 10.5/1000.
Doctors don’t have much negative risk in treatment. It isn’t their baby, it isn’t their money. Action is to their advantage, it may further their career if the action is relatively experimental. It may further their wealth if they are paid for procedures.
I believe all doctors I have ever met, and probably almost all doctors believe they are doing good. The pressure of this incentive system pushes slowly and gently toward more medical actions. It pushes common practice, the habit of treatment toward more procedures and more tests, regardless of their benefit to the patients.
I am not the first to suggest there is an issue. One indication of overtreatment is the rate at which doctors will cure themselves. Some studies indicate that doctors will undergo some procedures 1/2 to 1/5th as often as the general population. Why does the entire equation change when they have skin in the game? Would you bet the incentive structure is that different?
Would you bet your baby’s life?